Symptoms
What are the signs?
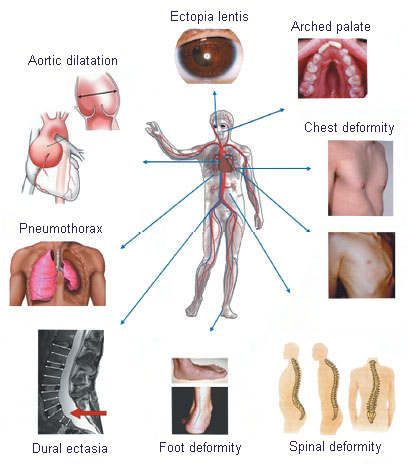
- Marfan syndrome can affect several parts of the body and each person is affected differently. The signs may even differ between members of the same family who have the same mutation.
- People are already born with MFS. Features may occur immediately or at a later age.
-
Many health problems get worse with age.
Cardiovascular system
Cardiovascular features occurs in 9 out of 10 patients with MFS. They are just the problems that threaten their lives.
The most serious problem is the widening of the aorta - the largest and most stressed vessel in the human body. In Marfan syndrome, the vessel wall is weakened, causing following problems:
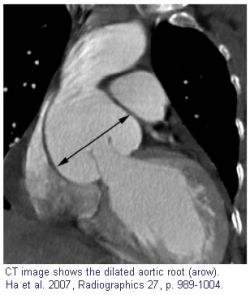
Aortic dilatation - enlargement of the aorta usually begins in the root - Valsalva sinus, but it can also occur in other parts of the aorta, aneurysm can occur. The doctor will determine if the aorta is dilated by evaluating diameter, age, height and weight. The risk of aneurysm is its tendency to rupture and subsequent bleeding, eventually depositing clots (thrombi) on the vessel wall and subsequent embolization. The aorta continues to expand with age.
Aortic regurgitation - the backflow of blood from the aorta to the heart, often results from aortic dilatation, which is so widespread that the valve cannot fully close.
The prolapse of a mitral valve is often the cause of regurgitation, so the valve does not close enough and blood leaks back. In some patients, this causes fatigue, weakness, heart palpitations, prickly pain, feeling a lack of air. Prolapse causes an increased risk of infectious endocarditis (in procedures such as tooth extraction, etc.).
Aortic dissection - is caused by tearing the inner wall of the aorta and
by passing of blood through a false channel between the inner and outer layers
of the aortic wall. It can affect all or part of the aorta length. A fatal
complication may be non-repletion of vital organs or aorta rupture and
bleeding.
Most people who have had aortic dissection
experience severe pain in the middle of their chest, abdomen (stomach), or
back. The pain may be "severe", "sharp",
"tearing" or "ripping" and may pass from the chest to the
back and / or the abdomen. Other symptoms may be present: pulse loss,
paraesthesia (tingling), paralysis, fainting. Sometimes, the pain is less
severe, but one still feels that "something is very bad."
In people with MFS, the risk of aortic dissection is 250 times higher than in the general population !!!
If a dissection is suspected, the patient must be promptly transported by emergency medical transport for urgent examination by one of the following methods:
- CT ( computed tomography)
- transesophageal echocardiography
- MRI ( magnetic resonance imaging)
ATTENTION: Normal X-ray examination does
not exclude the possibility of aortic dissection!
1) Dissection of the ascending aorta. It is the most common form of dissection in Marfan syndrome. The patient may die if mistreated. Usually, immediate operation is required. 50% of patients with undiagnosed aortic dissection die within 48 hours.
2) Dissection of descending aorta - in the thoracic or abdominal part. In most cases, monitoring and use of drugs is sufficient, surgery is required only in case of serious complications (loss of blood flow to the organs or severe dilatation of the aorta).
Because of the risk of spontaneous dissection, aortic (or possibly aortic valve) replacement surgery is recommended when the aortic root diameter reaches 50 mm, sometimes earlier, but each case is specific and must be assessed by a qualified cardiologist. Currently, there is a new method of attaching an external polymer mesh support to a portion of the aorta to stabilize the aortic wall and prevent further dilatation (Personalized External Aortic Root Support - PEARS).
EYES
A common sign (50-80% of cases) is dislocated lens of the eye. This is due to a change in the suspension apparatus of the lens, which is made up of the protein fibrillin. The complication is the complete tearing off of the lens, which can lead to other problems. Myopia is common. Sometimes detached retina occurs. In the case of severe pain (increase in intraocular pressure - glaucoma) it is a sudden event that needs to be treated immediately.
SKELETAL
Patients have disproportionately long and thin limbs and parts thereof. Characteristic are so-called spider fingers. A person with an MFS can wrap his wrist with his thumb and the little finger of his other hand, or his thumb protrudes from his clenched palm. Very often such people are characterized by a typical tall figure. The spine has a bad curvature (scoliosis / kyphosis), often the chest is deformed (inverted or chicken). There may be deformities in the foot, elongated head in the anterior-posterior direction and high-arched palate.
Hypermobility: A patient with MFS usually has excessive joint mobility beyond normal. The ligaments are weak and cause joint instability, which can lead to unexplained falls. Minor or major injuries are common and repeated in hypermobile people. Increased joint mobility makes them more susceptible to sprains, minor tears in tendon fibers and muscles; they are less powerful than in people without hypermobility. Some people have joint pain - so they have hypermobility syndrome. The pain can come directly from the joint, but it can also be located in the muscles and tendons. Virtually all joints, including spinal joints, can be affected. Muscle pain is where the muscles near the joint have to work more and harder because they compensate for excessive mobility of ligaments. With increased muscle work tendons are also stressed, causing pain.
Protrusio acetabulae: Incidence 16% - 27%. Acetabulum is the well of the hip joint. In
children with Marfan, the hole becomes deeper than normal during growth.
Although protrusio acetabulae does not cause problems in childhood or
adolescence, it can lead to painful forms of arthritis in adulthood (less than
5%). Changes of the hip joint reduce its mobility, unlike the hypermobility of
most other joints in the body.
LUNGS
Restrictive lung disease (the primary symptom is shortness of breath during exercise) in more than 70% of patients. Pneumothorax - spontaneous lung collapse occurs in about 10% of patients (symptoms are shortness of breath, dry cough, or acute onset of chest pain; pain worsens with deep breath). Emphysema - loss of alveolar walls and airway enlargement causes airway obstruction and inflammation. About 10-15 percent of people with MFS have lung emphysema, but it is probably underdiagnosed. Symptoms include dyspnoea in activity, frequent bronchitis and low oxygen content in the blood. Some people with MFS have sleep apnea - there are intervals (10 seconds to 3 minutes) during which the patient is not breathing during sleep.
NERVOUS SYSTEM
Dural ectasia - enlargement of the spinal cord, usually in the lower (lumbosacral) area, occurs in about 60% of patients. Detected by CT or MRI. The presence of ectasia may not always cause problems, although this sometimes causes aching in the very low back, almost in the tailbone, as well as abdominal pain, headaches, and leg pain. Pain and numbness in the perineum (the area between the legs in front of the anus) can also occur.
Please note: The information on this site does not substitute for professional healthcare. This is for informational purposes only and may not be used for treatment, prevention or diagnosis without first consultation with the physician.